Foot Conditions

Foot Conditions
Which Foot Conditions Can Be Treated at StrideCare?

Up to 70 percent of people will develop athlete’s foot in their lifetime. The fungus that causes it grows on the warm, damp surfaces around pools, public showers, and locker rooms. Athlete’s foot commonly occurs in people whose feet are sweaty and in tight-fitting shoes.
Symptoms of Athlete’s Foot
- Itchy, scaly rash between toes
- Small, red blisters
- Ongoing dryness and scaling
- Ulcers or sores



Flat feet are when the arches are flattened, allowing the entire soles of the foot to touch the floor when standing. Patients can be born with it or it can develop later in life. Many adults develop flat feet due to:
- Injury or trauma
- Rheumatoid arthritis
- Being overweight
- Chronic diseases, including diabetes
- Suddenly increasing the intensity, frequency, or duration of your exercise

There are 26 bones in the foot. Certain activities or injuries can cause a fracture or crack in one or more of these bones. Pain, redness, swelling, and bruising are signs of a possible fracture.

A foot ulcer is an open sore on the foot. More than any other group, people with diabetes have a particularly high risk of developing foot ulcers. This is because the long-term complications of diabetes often include neuropathy and circulatory problems. In addition to diabetes, atherosclerosis and Raynaud’s phenomenon increase the risk of foot ulcers.
When a patient experiences chronic pain in the foot and joints, podiatrists often prescribe orthotics. Orthotics are a medical device that helps alleviate foot pain caused by conditions such as plantar fasciitis and rheumatoid arthritis and are designed to correct biomechanical foot issues such as how to walk, stand, or run.
Over time, the protective cartilage that cushions the ends of the bones as they move wears down and not only restricts the ability to perform daily activities but also causes damage to joints in the hands, knees, hips, and spine. Osteoarthritis can occur in a person’s big toe, midfoot, and ankles.
Osteoarthritis is considered a wear-and-tear disease. The symptoms develop slowly and get worse over time. Though certain treatments can make osteoarthritis easier to manage, damage to the joint is irreversible.

The plantar fascia is a thick band of tissue that runs across the bottom of the foot and connects the heel bone to the toes. Plantar Fasciitis is painful inflammation of that tissue. It is caused by repetitive strain from excessive running or walking, repeated jumping, and inadequate shoes. While Plantar Fasciitis can develop without an obvious cause, podiatrists see higher incidences among runners and people who are constantly on their feet. The pain is worse first thing in the morning and after the activity, not during it.

Rheumatoid Arthritis affects over 1.3 million Americans. It is characterized by painful inflammation of one or more joints, including the feet, and causes stiffness that only worsens with age. The average person doesn’t typically experience symptoms until they are in their 60s. Podiatrists tend to see more women than men for cases of rheumatoid arthritis, which can feel like a sprain or broken bone and, in some cases, may be painful to the touch.

Plantar warts are small growths with a rough texture that grow on the heels, soles, or any other area of the foot. They are not life-threatening and can go away over time without medical treatment, but they tend to be painful and will likely multiply if left untreated. Warts enter the skin through a cut on the bottom of the foot and are more common in children, teenagers, and people with a weakened immune system. People who walk barefoot—especially at public swimming pools or in locker rooms and communal showers—are also susceptible. Patients need to see a podiatrist if the wart is large, there are several of them, or if they are causing discomfort.
More than just treating a standard cut or scrape, wound care is a specialized medical protocol that involves treating wounds that do not heal and are likely the result of a more serious underlying condition. Wounds are typically considered non-healing if they have not started to heal in two weeks or have not completely healed in six weeks. Examples of non-healing wounds include foot ulcers due to diabetes, venous insufficiency, or swollen legs.
It is essential that people with diabetes care for their feet and regularly visit with a podiatrist to reduce the risk of slow-healing wounds and complications. This includes foot ulcers, lower leg ulcers, pressure ulcers, surgical wounds, lacerations, infections, and more.
Neuropathy affects roughly 20 million people in the United States. It occurs when nerves that carry messages to and from the brain and spinal cord to the rest of the body are damaged. It is associated with a litany of underlying medical conditions and affects a single peripheral nerve or several nerves at the same time.
FIND A
CONVENIENT LOCATION
StrideCare Leverages athenaOne to Enhance Financial and Operational Results, Improve Clinical Workflows
2 Min ReadCASE STUDY: Transitioning all practices onto one united system gives StrideCare invaluable access to data

When are Varicose Veins More than Just a Cosmetic Concern?
2 Min ReadLearn about varicose veins, prevention tips, and treatment options from StrideCare’s vein specialists in Texas.
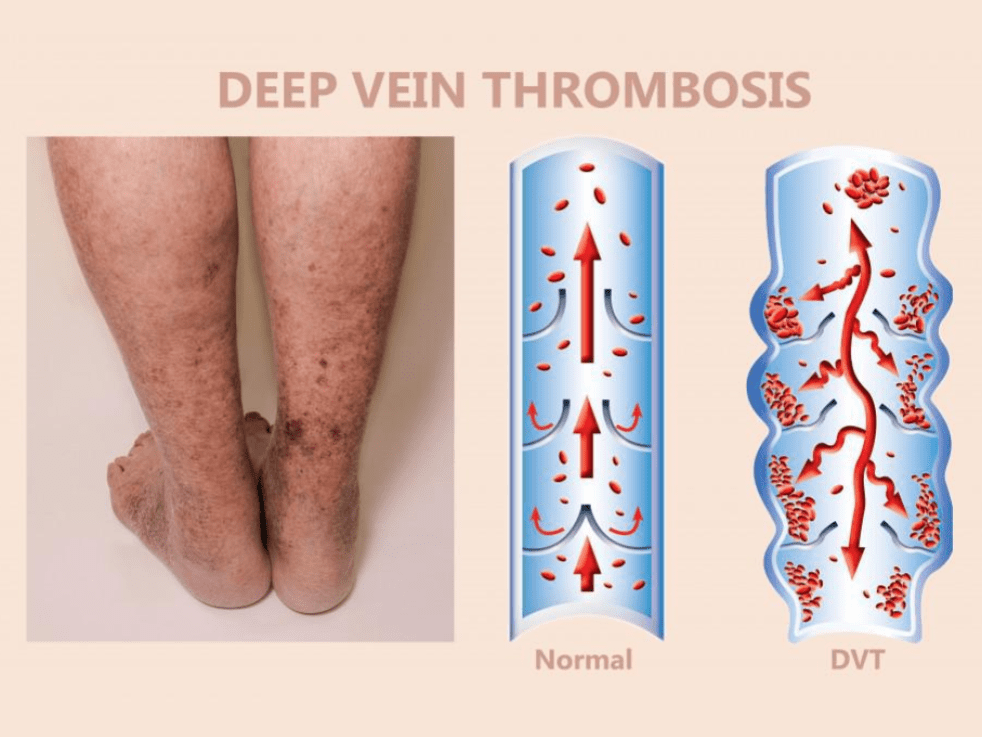
Puffy Legs are One of the First Signs of Deep Vein Thrombosis
3 Min ReadLearn the symptoms of deep vein thrombosis (DVT) and seek immediate evaluation at StrideCare for expert care and treatment.