Do I Have a Blood Clot? Signs of Deep Vein Thrombosis You Shouldn’t Ignore
Author: StrideCare Internal Team
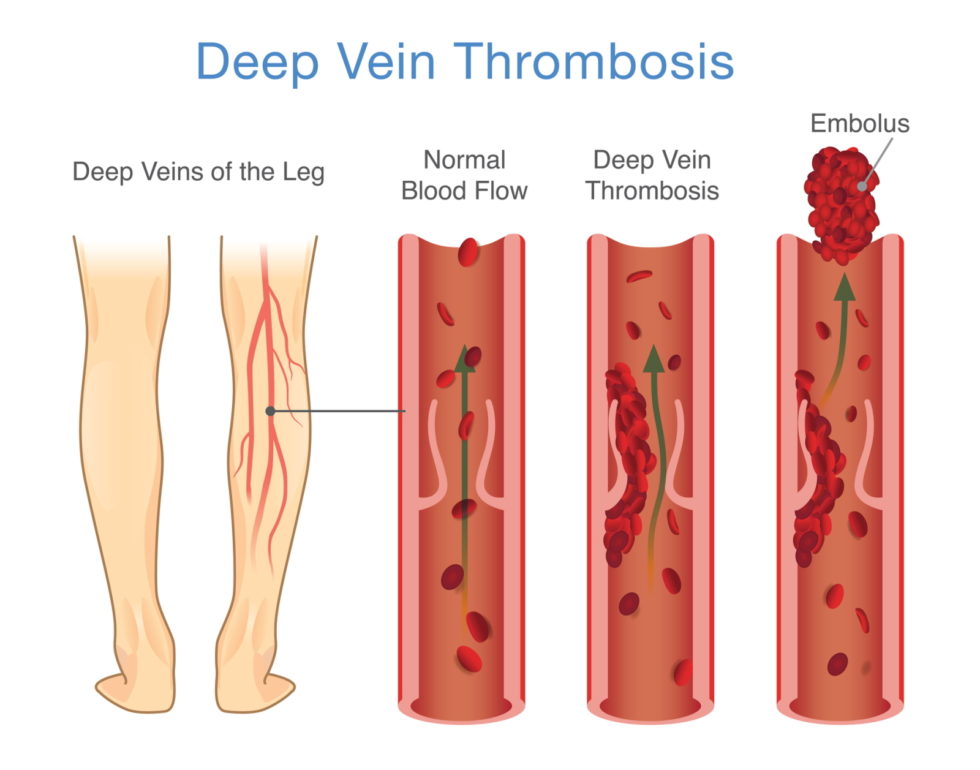
If you’ve noticed swelling, pain, or redness in your leg, you might be wondering: could it be a blood clot? These are often signs of a condition called deep vein thrombosis (DVT), a potentially serious vascular issue.
Michael* was an avid marathoner, including having competed in the Chevron Houston Marathon. But last year he began experiencing calf pain, and his right leg was swollen and warm to the touch. The most troubling part, though: he ignored the pain. He was young and never had health issues before, so he assumed symptoms were from pushing too hard with his training routine. Just a temporary setback, he thought. But the symptoms didn’t improve, and it wasn’t until three days later that he went to the doctor and was diagnosed with a leg blood clot—also known as vein thrombosis.
Thankfully, Michael recovered and is back to doing what he enjoys. But he’s a perfect example of how quickly and unexpectedly blood clots can impact a person’s life—even someone like Michael, who is otherwise healthy and in peak condition. Up to 600,000 people in the United States each year are impacted by vein thrombosis, and up to 100,000 people die yearly. The first steps to overcoming this condition are being educated about what deep vein thrombosis is, knowing if you have one, and scheduling an appointment with Stridecarefor a proper diagnosis.
Symptoms of Deep Vein Thrombosis (DVT):
Swelling in one leg
Pain or tenderness, especially in the calf
Warmth or redness on the skin
A heavy or aching feeling in the leg
- Burning sensations in the feet
How to Know If You Have Deep Vein Thrombosis
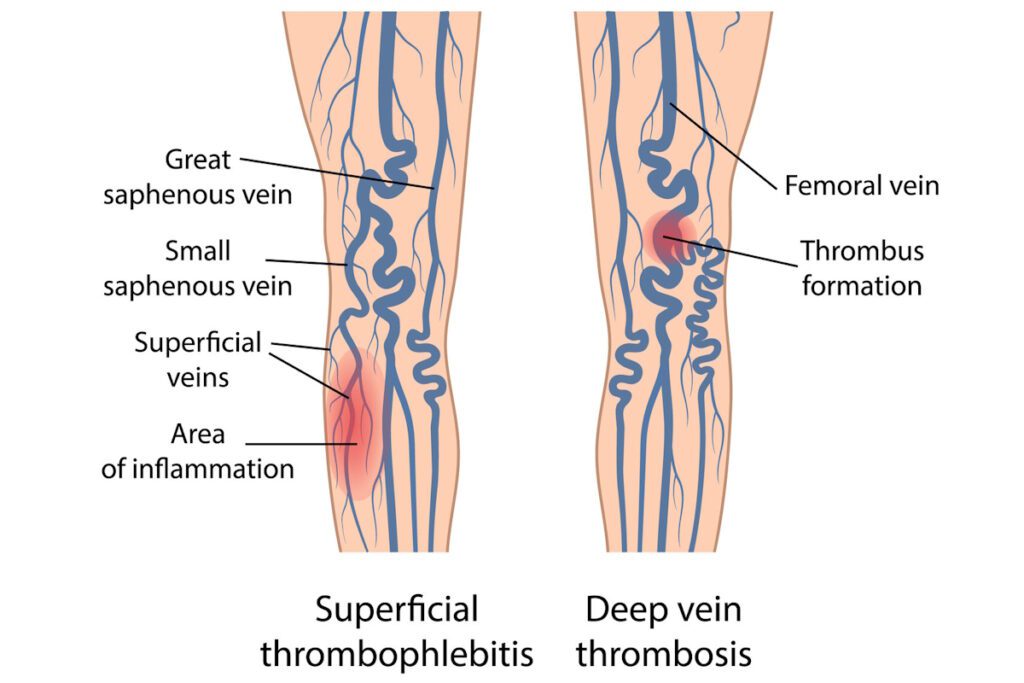
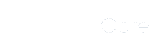
Essentially a blood clot occurs when blood that is meant to be flowing freely inside your veins and arteries becomes too sluggish and begins to clot. These blood clots can either create a partial or complete blockage, and you experience an immediate decrease in blood circulation. Vein thrombosis by itself is not life-threatening, but any blood clot can break free and travel through your bloodstream. If left untreated, or if it develops into a DVT, a blood clot can lead to strokes, pulmonary embolisms, heart attacks, and even death.
If you are experiencing any of the symptoms above, it’s much easier to recognize that you might have deep vein thrombosis. Yet, the symptoms aren’t the same for everyone, and some people don’t experience any symptoms or pain at first. This makes it even more difficult to stay on top of your health situation.
If this is the case for you, it’s important to be more aware of your risk factors. These can include the following:
- Lack of mobility — Blood slows down and becomes sluggish when the body isn’t moving. Examples of situations where lack of mobility can become a problem include long car or plane rides, working conditions where you’re forced to sit for long stretches, being bedridden due to injury or illness, and leading a sedentary lifestyle.
- Dehydration — A lack of water and fluids in general increases the risk of vein thrombosis because it makes the blood thicker, thus slowing down blood circulation.
- Surgery or injury — Injuries happen, and surgeries are necessary for many circumstances. But when they limit your ability to move around, or your veins were damaged because of surgery or injury, blood clots form. Debris, tissue, and even collagen could release into your bloodstream and make the blood around those particles thicker.
- Pregnancy — When a woman is pregnant, her blood tends to clot more easily to lessen blood loss during delivery. Prolonged immobility is also an issue, especially after a C-section. Pregnant women may also experience vein thrombosis because the blood vessels around the pelvis are chronically pressed upon by growing the baby.
- Medications — Birth control pills, painkillers, and non-steroidal anti-inflammatory drugs such as aspirin or ibuprofen can promote blood clotting and are an all-too-real concern for developing deep vein thrombosis.
- Smoking — Smoking damages the lining of blood vessels, leads to higher risks of vascular disease, and raises the risk of unwanted vein thrombosis.
- Inherited blood-clotting disorders — People with inherited conditions tend to develop blood clots before 45 years of age and without a specific cause. These same people are likely to have more than one blood clot in their lifetime.
Is Deep Vein Thrombosis Preventable or Treatable?
In a word—yes. You can improve your odds of not getting vein thrombosis by staying active as much as possible, eating healthy, and avoiding a sedentary lifestyle. Even when you’re at work or stuck on an airplane flight, you should attempt to get up and walk around every 1 or 2 hours, raise and lower your heels, and wear loose-fitting clothing. If you are already at risk for blood clots, your doctor can prescribe compression socks to promote increased blood flow.
If you suspect that you have deep vein thrombosis, treatment is always an option and is typically highly successful when the condition is caught early. If the area is swollen or painful, your provider may recommend that you first:
- Elevate your leg.
- Apply a warm compress to the area.
- Take nonsteroidal anti-inflammatory drugs (NSAIDs).
- Wear compression stockings.
StrideCare is a premier center for properly diagnosing DVT through diagnostic venous ultrasound or a venography. This allows us to recognize vein disease at all stages and dramatically improve our patients’ quality of life.
Diagnostic Venous Ultrasound
Uses sound waves to view the circulatory system and structures of the veins underneath the skin to search for blood clots. It is typically the first exploratory option, and the process takes 45-60 minutes to complete, and there is no cutting, scarring, or anesthesia. You’ll be able to return to your normal daily activities immediately after the procedure, including work.
Venography
This test can uncover problems with veins that venous ultrasound cannot view. With venography, a provider will inject an iodine-based solution into the veins to act as a contrast that can be seen easily on an x-ray. You may experience some mild bruising and tenderness, but this is normal.

StrideCare Can Diagnose and Relieve Leg Swelling Issues
Vein thrombosis can affect anyone at any age and can impact individuals who are active and those who lead sedentary lifestyles. Blood clots can also cause no pain at all until it’s too late or a variety of telltale symptoms ranging from swelling in the legs and feet to skin discoloration, shortness of breath, and chest pain. If you experience any changes in the look, feel, and condition of your legs, please do not hesitate to visit a trained professional. These and other conditions can get worse and lead to more complicated symptoms.
Our expert doctors and highly skilled team members at StrideCare are proud to offer treatment for a variety of vein and artery diseases that might dramatically impact your quality of life. We only utilize the latest technologies and minimally invasive procedures. Procedures take place at in-office or outpatient settings. Patients suffering from a multitude of vascular conditions that include venous insufficiency, varicose veins, spider veins, diabetic vascular disease, venous ulcers, peripheral artery disease, leg discoloration, lymphedema, restless legs syndrome, and more can benefit from these minimally invasive treatments.
Prior to starting any new treatment or questions regarding a medical condition, always seek the advice of your doctor or other qualified health provider. This information is not a substitute for professional medical advice.
StrideCare serves the South Texas area including Houston, San Antonio, Austin, Round Rock, Bastrop, Brushy Creek, Cedar Park, Converse, Georgetown, Hutto, Kyle, Leander, Marble Falls, New Braunfels, Pasadena, Pearland, Pflugerville, San Marcos, Schertz, Houston, Sugar Land, Katy, Webster, Bay City, Clear Lake, Lake Jackson, The Woodlands, Universal City, Spring, Kingwood, Stafford, Conroe, Texas City, Cypress, League City, Bellaire, and more.
*Patient stories are true. Names and/or photos may be changed to protect patient confidentiality.