Peripheral Vascular Disease: Is Balloon Angioplasty Right for Me?
Author: StrideCare Internal Team

Emilio’s* elderly mother was recently diagnosed with peripheral vascular disease (PVD), a common circulatory condition that affects approximately 6.5 million people over the age of 40 in the United States. While treatable, PVD can become a life-threatening condition if ignored, misdiagnosed, or left unchecked. As a result, Emilio feels as if there isn’t any time to waste and has been spending his days lately trying to figure out what the best treatment option is without surgery, with one of them being balloon angioplasty. But is balloon angioplasty the right option for his mom’s unique situation?
The quick answer is, “it depends.” A consultation with his mother’s specialist at Stridecare can determine the severity and location of her PVD symptoms. If she is a good candidate, balloon angioplasty will likely be the best course of action.
For anyone suffering from peripheral vascular disease, the key is not to delay seeking help. If you delay, the condition and the symptoms you or your loved one are experiencing may worsen over time.
What is Peripheral Vascular Disease?
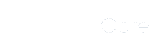
Our veins and arteries are a very intricate and interconnected web of networking that allows blood to flow properly to and from the heart and throughout our body. Over time, our arteries can develop a buildup of plaque. These blockages or narrowing drastically limit blood flow.
PVD, also referred to as arteriosclerosis of the extremities or peripheral artery disease, is characterized by poor blood circulation to the kidneys, intestines, arms, legs, and feet—leading to tissue and nerve injury or damage.
PVD can lead to a variety of symptoms, including:
- Painful cramping in the legs or hips
- Changes in the appearance of extremities (color, loss of hair, shiny skin)
- Cold legs and feet
- Open sores that don’t heal
- No pulse or weak pulse in legs and feet
The Centers for Disease Control say that up to 4 in 10 people with PVD don’t have symptoms, but sluggish blood flow can quickly progress from no symptoms to varying degrees of pain in one or both legs. If left unchecked, PVD symptoms can lead to a critical state of “no blood flow.” And if this happens, you could be at risk for leg amputation.
There are various causes of peripheral vascular disease including:
- Smoking — Up to 80% of patients with PVD are current or former smokers.
- Diabetes — Roughly 20-30% of people diagnosed with PVD also have diabetes.
- Obesity — People who are obese are 1.5 times more likely to develop peripheral vascular disease.
- Cardiovascular disease — Any condition that affects the heart or blood vessels is likely to be associated with PVD.
- High blood pressure — You can prevent PVD and improve symptoms by lowering your blood pressure
Tell Me About Balloon Angioplasty
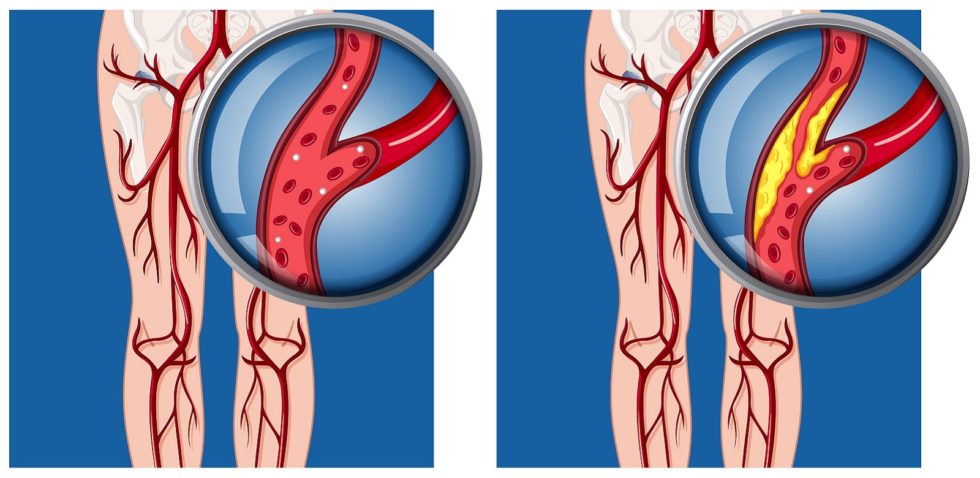
Balloon angioplasty is often recommended to patients who have peripheral vascular disease. It is extremely popular because it doesn’t involve a lengthy and complex surgery. With this minimally invasive procedure, your vascular specialist inserts a balloon attached to a small catheter into the body through a small incision in an artery. The catheter is then advanced to the affected artery, and a balloon system is inflated several times. By inflating it numerous times, the balloon widens the passage and lets blood flow freely.
In many situations, a tubular device called a stent is then inserted into the artery to ensure the blood vessel remains open long-term. The goal, obviously, in treating peripheral vascular disease is to restore blood flow in a clogged artery while at the same time increasing oxygen-rich blood delivery throughout the body’s muscles and tissues. It is not a 100% cure for blocked arteries, and it is possible that some patients may experience a re-narrowing of arteries as plaque builds up again. Therefore, using angioplasty in conjunction with stunting can provide longer-lasting results.
As for pain associated with this procedure, you may experience some mild bruising and tenderness at the access site immediately following balloon angioplasty. But this is normal and typically resolves on their own within a few days of treatment. Your specialist will provide you with detailed postoperative instructions before your angioplasty so that you know what to expect.
Balloon angioplasty differs slightly from two other minimally invasive treatments for peripheral vascular disease, atherectomy and stenting. Below is a brief description of each:
Atherectomy
This procedure uses advanced laser technology to clear away plaque and buildup on large blood vessels, including the coronary artery, which is responsible for bringing oxygenated blood to the heart. You might hear the word laser and think surgery but in reality, an atherectomy is also minimally invasive and is typically combined with balloon angioplasty and stunting.
Stenting
As previously mentioned, stenting involves using a mesh tube to keep a closed-off blood vessel open for the longer. It is performed with angioplasty so that the balloon can open the artery up and clear out any buildup before the stent is placed. This is a relatively gentle procedure that ensures blockage cannot reoccur.
StrideCare Is Your Specialist for Balloon Angioplasty
You don’t need to continue suffering from peripheral vascular disease. Our expert doctors and caring staff at StrideCare utilize the latest technologies and minimally invasive procedures to help our patients with a variety of vein and artery diseases. The vascular physicians at StrideCare are board-certified diagnostic radiologists with additional fellowship training in vascular and interventional radiology.
Prior to starting any new treatment or questions regarding a medical condition, always seek the advice of your doctor or other qualified health provider. This information is not a substitute for professional medical advice.
StrideCare serves the South Texas area including Houston, San Antonio, Austin, Round Rock, Bastrop, Brushy Creek, Cedar Park, Converse, Georgetown, Hutto, Kyle, Leander, Marble Falls, New Braunfels, Pasadena, Pearland, Pflugerville, San Marcos, Schertz, Houston, Sugar Land, Katy, Webster, Bay City, Clear Lake, Lake Jackson, The Woodlands, Universal City, Spring, Kingwood, Stafford, Conroe, Texas City, Cypress, League City, Bellaire, and more.
*Patient stories are true. Names and/or photos may be changed to protect patient confidentiality.