How to Recognize and Reduce Edema (Water Retention)
Author: StrideCare Internal Team

Kathy* has experienced swelling and water retention before. Thankfully, none of those episodes—usually a result of an allergic reaction to medication or a bug bite—were serious and quickly resolved themselves. But this time is different. There’s seemingly no rhyme or reason for it, and the swelling isn’t going away. On top of that, she has muscle cramps and a constant achy and heavy feeling in her legs. After months of finding zero relief with at-home treatments and rest, her doctors diagnosed her with edema. More importantly, they referred her to a vascular specialist to see if her edema and discomfort resulted from a much bigger issue.
We’ve all experienced temporary swelling and water retention at some point in our lives. But edema is a much more serious condition and could be a sign that vein disease is to blame. More than 20 million Americans suffer from some form of vein disease. If you’re experiencing chronic edema in your legs and feet, this can be the reason. Ignoring one or both issues could worsen your symptoms and significantly impact your quality of life.
Are You Experiencing Any of Symptoms with Edema?
- Swelling in one or both legs that can come and go
- Achy or heavy feeling in your legs
- Cold and numb feet
- Skin that retains a dimple after being pressed for several seconds
- Stretched or shiny skin
- Limited range of motion
- Burning, throbbing, and itching
- Muscle cramps
- Fainting or dizziness
- Discomfort after sitting or standing for too long
- Pain when walking
- Skin discoloration and thickened skin
- Open sores and ulcers on your legs

What Causes Edema and Water Retention?
Edema is a term used to describe chronic and excess fluid in your body’s tissues that are trapped and can’t be released. Patients with edema typically notice it more in their legs, feet, and ankles, though it can affect any part of the body. It can also affect anyone but is usually more common in people who are pregnant and adults over 65.
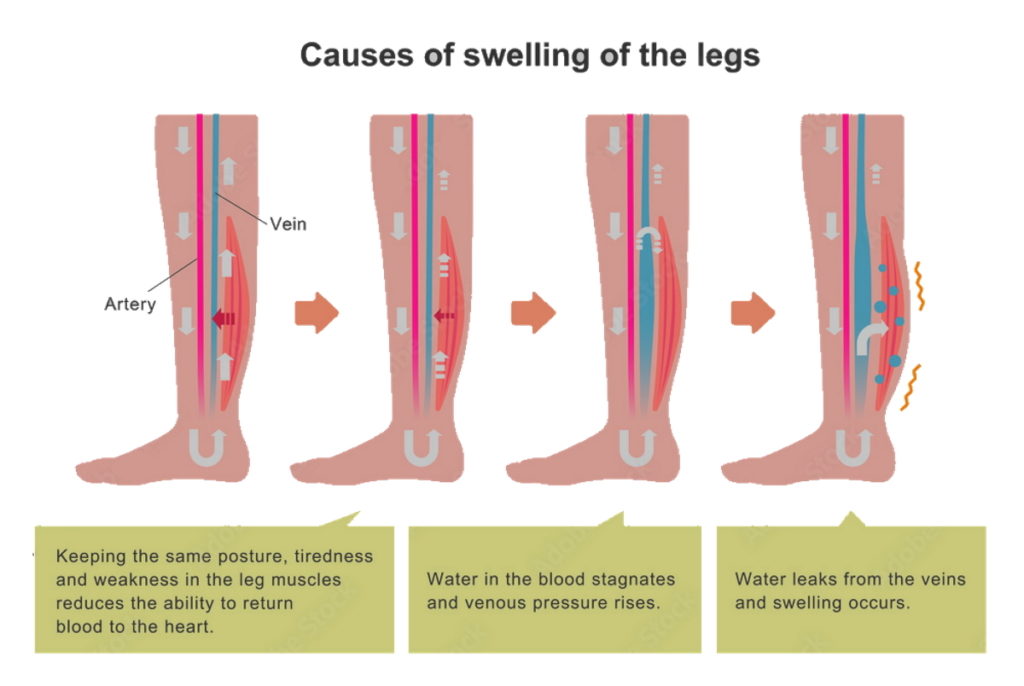
There are many reasons you may suffer from edema that are not necessarily due to vein disease. For example, you could have just completed a long airplane flight with limited opportunities to get up and move around. When you wake up the next day, one leg or foot is larger and more swollen than the other. Consistently sedentary lifestyles, pregnancy, eating too much salt, and even certain medications can also cause excess swelling. But for others, vein disease could be the culprit. And here’s why:
Our veins are a super intricate web system responsible for carrying blood back to the heart to support many systems critical to our cardiovascular health and other functions. As we age, vein valves can weaken and become diseased. As a result, blood isn’t pumped throughout the body as efficiently as it once was. As water leaks from the veins, fluid retention accumulates, and pressure builds up, swelling is bound to occur.
A few examples of vein conditions that can cause chronic leg swelling or edema include:
Varicose Veins
Varicose veins are extremely common and affect roughly 25% of men and women in the United States. This is a condition where the veins stop working properly, fill up with blood, and enlarge or swell due to a high volume of fluid buildup. This can cause leg swelling and edema.
Lymphedema
Lymphedema is slightly different from edema in that it describes a condition where the lymph nodes in your body aren’t draining excess fluids from your tissues. As a result, there is a buildup of lymph fluid in the fatty tissues just under your skin that causes chronic swelling that comes and goes.
Chronic Venous Insufficiency (CVI)
CVI is a condition in which broken valves do not hold a seal and causes blood pressure to build up in the lower legs. This results in pooling of the blood called venous stasis, leading to swelling and skin changes. Advancing age, family history, prolonged standing, obesity, smoking, sedentary lifestyle, and pregnancy are all considered risk factors.
Deep Vein Thrombosis
Swelling on only one leg is perhaps the most worrisome sign that your edema could be related to a very serious vein disease called DVT. This is where blood clots form in one of the veins deep within your body, causing fluid and blood to become trapped with no ability to escape. Up to 100,000 people die each year from deep vein thrombosis.
How Can I Reduce My Edema Symptoms?
The good news is that edema is treatable through lifestyle changes and minimally invasive treatment options from your vascular specialist. A few conservative options include:
Wear compression socks — Compression socks apply gentle pressure to improve circulation, reduce edema, and help support painful legs during long work shifts, plane flights, and standing on your feet for a long time.
Eat better — A better diet (fruits, vegetables, foods high in Vitamin C and E, and fiber-rich foods) promotes blood circulation and improves cardiovascular health.
Avoid tight clothing — Blood flow can be restricted by clothing that’s tight in the waist, legs, and upper thighs. As a result, chronic swelling and edema can set in.
Elevate your legs — Doctors suggest that elevating your legs above your heart at least three times a day for 15 minutes each time allows gravity to aid in creating more blood flow and decreasing edema symptoms.
Exercise — Staying active, exercising, and avoiding a sedentary lifestyle improves blood flow in the body.

If these methods don’t work, quick and easy procedures can be performed without the need for leg surgery. To determine the cause of your edema, our expert vein doctors at StrideCare will use the latest ultrasound equipment to get an inside look at your vascular system and how it is performing. Depending on your diagnosis and if the cause of your edema is vein related, we will determine the most effective treatment option for you.
StrideCare Is Your Edema Expert
Edema is a frustrating condition that no one should have to live with. Occasionally, the reasons for this water retention are minor and will improve on their own with conservative treatment and a few lifestyle changes. However, chronic leg swelling issues are better off being looked at by a trained vascular specialist. Early intervention for something that doesn’t seem very serious at first can help avoid painful symptoms such as tired and heavy legs, as well as eliminate the threat of life-altering blood clots, etc.
Our expert doctors and caring staff utilize the latest technologies and minimally invasive procedures to help our patients with a variety of vein and artery diseases. Our physicians are board-certified diagnostic radiologists with additional fellowship training in vascular and interventional radiology.
With multiple locations in D/FW, StrideCare has long been a leader in North Texas, performing leading-edge procedures to treat venous disease such as chronic venous insufficiency, varicose veins, spider veins, restless leg syndrome, pelvic congestion syndrome, iliac vein stenosis and more—all the while providing compassionate patient care.
If you have questions about edema or are experiencing leg pain, the experts at StrideCare will recommend an individualized plan to help you get the best results.
Prior to starting any new treatment or questions regarding a medical condition, always seek the advice of your doctor or other qualified health provider. This information is not a substitute for professional medical advice.
StrideCare serves the South Texas area including Houston, San Antonio, Austin, Round Rock, Bastrop, Brushy Creek, Cedar Park, Converse, Georgetown, Hutto, Kyle, Leander, Marble Falls, New Braunfels, Pasadena, Pearland, Pflugerville, San Marcos, Schertz, Houston, Sugar Land, Katy, Webster, Bay City, Clear Lake, Lake Jackson, The Woodlands, Universal City, Spring, Kingwood, Stafford, Conroe, Texas City, Cypress, League City, Bellaire, and more.
*Patient stories are true. Names and/or photos may be changed to protect patient confidentiality.