Can May-Thurner Syndrome Be Cured?
Author: StrideCare Internal Team

Becky* was young, healthy, and active. And yet, there she was sitting in the hospital as a doctor explained that she had a deep vein thrombosis (DVT), or blood clot, in her left leg, which was now heavy and swollen. At first, no one knew the exact cause, but it was determined later that the underlying culprit was a rare and often overlooked condition known as May-Thurner Syndrome. Naturally, her next question was, “Can May-Thurner Syndrome be cured?”
The good news is that Becky recovered nicely and is back to being her usual self. But things could have been much worse. People with May-Thurner Syndrome typically don’t have any symptoms, making it nearly impossible to diagnose until they develop dangerous blood clots that could have life-altering consequences.
Are You Experiencing Any of These Symptoms?
- Pain and swelling in the left leg
- Pain that feels like a charley horse or cramp
- A feeling of heaviness or throbbing in the leg
- Skin discoloration
- Pain in the lower abdomen and pelvis
- Skin that’s warm to the touch
- Enlarged veins in the leg
- Open sores on the leg
The Connection Between May-Thurner Syndrome and DVT
Your blood vessels and arteries work together to carry blood to and from your heart and throughout your body. This interconnected network of arteries and veins naturally cross over each other. But every so often, the right iliac artery, which carries blood to your right leg, puts pressure on and compresses the left iliac vein, which is responsible for carrying blood out of your left leg and toward your heart. This is called May-Thurner Syndrome, also known as iliac vein compression syndrome. If this happens, it can cause a blockage of blood flow.

As a result, MTS can cause deep vein thrombosis, a very serious condition characterized by all of the symptoms above. If a DVT breaks off and travels to your lungs, it can lead to a pulmonary embolism, heart attack, or stroke.
May-Thurner Syndrome occurs in young women between the ages of 20 and 45 more than men. It is also rare and hard to diagnose because it usually doesn’t have symptoms. With that said, roughly 18-40% of those who develop DVT can attribute it to May-Thurner Syndrome.
What Causes May-Thurner Syndrome?
You can be healthy and active and still get May-Thurner Syndrome. But you are more likely to get it if you:
- Have been pregnant in the past
- Regularly take birth control
- Have scoliosis
- Are inactive for long periods of time
- Had previous surgery or infection
- Are dehydrated
- Are susceptible to blood clots
How Is May-Thurner Syndrome Diagnosed?
There are no standardized criteria to establish a diagnosis for MTS, though those with DVT in the left leg typically have it. Your doctor will first do a thorough exam and look for symptoms of DVT, and imaging such as an MRI, CT, Ultrasound, or Venogram will show the veins in your leg and help identify signs of May-Thurner Syndrome.
From there, the goal is to treat the clots you do have. While there is no cure for May-Thurner Syndrome, the good news is it can be treated successfully to relieve symptoms. Your treatment will depend on your symptoms and risk factors. Below are a few procedures a physician will consider:
- Blood thinners and other medication — Anticoagulants reduce the blood’s thickness, allowing it to pass through compressed or damaged veins and arteries easier. They are also good for preventing new clots from forming.
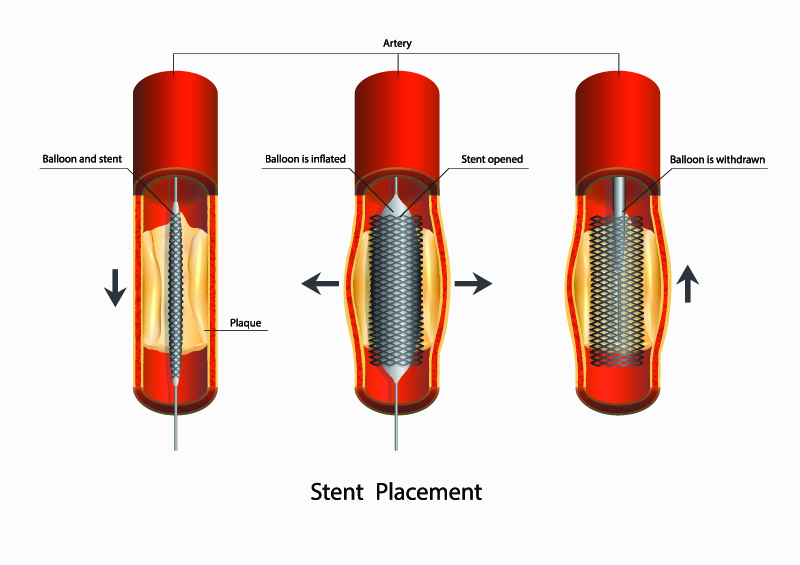
- Angioplasty and a stent — With angioplasty, your doctor will use a balloon system to open up the diseased artery and clear plaque build-up from the artery’s walls. A stent is also recommended. A small mesh tube is used to keep a closed-off or compressed blood vessel open for the long term.
- Atherectomy — Laser technology that clears plaque build-up on blood vessels. It can be performed on its own but is often combined with angioplasty and a stent.
- Bypass surgery — This procedure is considered for extreme cases of May-Thurner Syndrome and DVT. The goal is to reroute blood from the compressed vein with a bypass graft.
Results of treatments for MTS are generally very good. If identified shortly after the DVT has formed, most patients can receive treatment with complete resolution of symptoms.
Turn To StrideCare for Help with May-Thurner Syndrome
While it is difficult to diagnose May-Thurner Syndrome because of a lack of symptoms, it can be the culprit behind many patients who have DVT. If you experience any changes in the look, feel, and condition of your legs, please do not hesitate in visiting a trained professional. These and other conditions will get worse and lead to more complicated symptoms.
StrideCarehas long been a leader in performing leading-edge procedures to treat vein disease, and we are here to help you. The vascular physicians at StrideCare are board-certified diagnostic radiologists with additional fellowship training in vascular and interventional radiology.
The experts at StrideCare will recommend an individualized plan to help you get the best results. Request an appointment for a vein disease evaluation to discuss your options.
Prior to starting any new treatment or questions regarding a medical condition, always seek the advice of your doctor or other qualified health provider. This information is not a substitute for professional medical advice.
StrideCare serves the South Texas area including Houston, San Antonio, Austin, Round Rock, Bastrop, Brushy Creek, Cedar Park, Converse, Georgetown, Hutto, Kyle, Leander, Marble Falls, New Braunfels, Pasadena, Pearland, Pflugerville, San Marcos, Schertz, Houston, Sugar Land, Katy, Webster, Bay City, Clear Lake, Lake Jackson, The Woodlands, Universal City, Spring, Kingwood, Stafford, Conroe, Texas City, Cypress, League City, Bellaire, and more.
*Patient stories are true. Names and/or photos may be changed to protect patient confidentiality.