Diabetic Vascular Disease a Focus of National Diabetes Month
Author: StrideCare Internal Team

Diabetes being a huge topic of discussion, especially as we turn our attention to National Diabetes Month in November. Even so, the reality is that many of the 100 million diagnosed patients worldwide are also at risk of developing diabetic vascular disease. Yes, common symptoms of diabetes that everyone knows include excessive weight loss and fatigue, urinary frequency, blurry vision, and increased hunger and thirst. But diabetic patients must also be on the lookout for arterial irregularities and changes in the appearance of their legs and feet.
At StrideCare, we believe in promoting education and awareness efforts such as National Diabetes Month. This is even more crucial as it relates to patients’ ability to recognize a litany of vascular and arterial diseases. These changes are your body’s way of telling you something is wrong. Ignore them, and you could drastically impact your quality of life.
Do You Have These Symptoms of Diabetic Vascular Disease?
- Pain in your legs when walking
- Wounds that won’t heal over pressure points, such as heels or ankles
- Burning sensation in your hands, feet, or toes
- Foot ulcers or sores on your feet
- Numbness, weakness, or heaviness in muscles
- Loss of feeling in your hands or feet
- Shiny skin or skin color changes
- Loss of leg hair
- Thickened, opaque toenails
- Coldness in the lower leg or foot
- No pulse or a weak pulse in the legs or feet
- Swelling or unexpected weight gain in your face or limbs
- Restricted mobility
- Foamy looking urine
- High blood pressure
- Blurry vision and/or floating spots in your vision
- Chest pain
The Importance of National Diabetes Month
Approximately 37.3 million Americans have diabetes, and more than 1 in 3 adults have pre-diabetes. That’s 88 million people with pre-diabetes alone. Unfortunately, most people don’t know they have it. But what is diabetes? This disease is characterized by the body’s inability to produce or properly use insulin, a regulator of glucose in the blood.

There are two main types of diabetes you could be diagnosed with:
Type 1 diabetes
An autoimmune disorder that predominately affects children and adolescents. Approximately 1.25 million Americans have Type 1 and must take insulin injections to survive because the insulin-producing beta cells in their pancreas have been destroyed. Type 1 diabetes is usually hereditary.
Type 2 diabetes
Type 2 diabetes accounts for 90 to 95% of all diabetes. The biggest difference is that while the pancreas is still producing insulin, it doesn’t produce enough, or the patient is becoming insulin resistant. Type 2 diabetes is the one that has more symptoms that could be a sign of diabetic vascular disease, including sores or cuts that won’t heal and areas of darkened skin.
National Diabetes Month and World Diabetes Day on November 14 are the perfect vehicles to spur communities, everyday individuals, and healthcare officials across the country to bring awareness to diabetes, its symptoms, and its connection with diabetic vascular disease. In fact, the theme of this year’s World Diabetes Day is “education to protect tomorrow.” The International Diabetes Foundation has launched a global survey to explore the levels of access that healthcare professionals and people living with diabetes have to diabetes education.
The survey can be found here. Answers will be used to inform World Diabetes Day 2022 activities and highlight the importance of accessible and quality diabetes education to protect tomorrow.
Diabetes and Diabetic Vascular Disease Conditions
Anyone can be diagnosed with a vascular disease, but as stated earlier, diabetic patients are at a higher risk because of the way the disease can damage the arteries. Below is a breakdown of a few vascular diseases that can present themselves in diabetic patients.
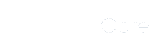
Peripheral Arterial Disease (PAD)
PAD, also known as arteriosclerosis, affects 8.5 million U.S. adults and 113 million people worldwide. It is a diabetic vascular disease characterized by plaque buildup on the walls of the major blood vessels or arteries. When this plaque is allowed to build up, it creates narrower openings for blood and oxygen to pass through. And, yes, too much restricted blood flow or a complete blockage to the extremities can cause pain or lower leg tingling sensations.
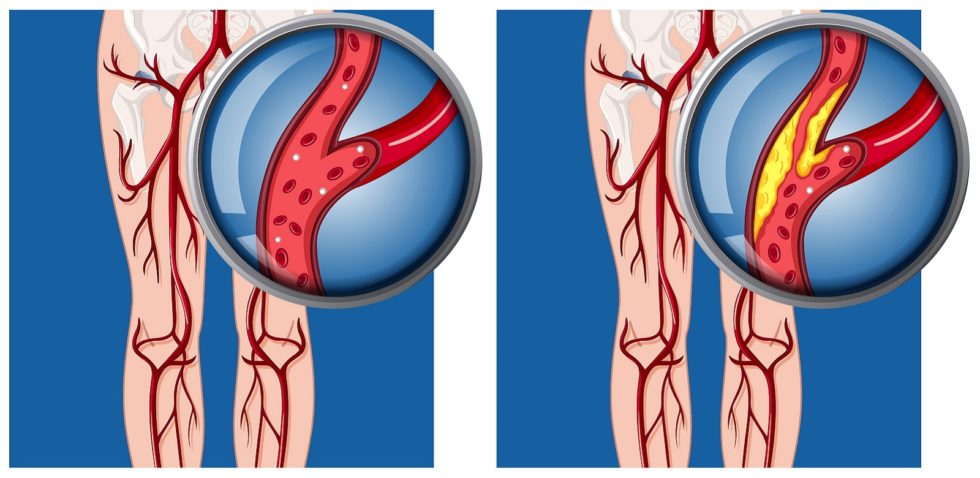
Diabetic Foot Ulcer
Patients with diabetes are more susceptible to foot problems due to complications from the disease. One of the most common foot problems for diabetic feet are foot ulcers. These are caused by blocked or clogged arteries. Their location is so on outer side of the ankles, feet, heels, and toes. Telltale signs are:
- Skin discoloration
- Leg pain that worsens as you stand
- Scabbing, flaking, thickening, or itchy skin
If left untreated, these ulcers can become infected and, in the worst-case scenario, the toes and/or foot will require amputation. However, with the right diabetic foot care, ulcers and infections can be prevented.
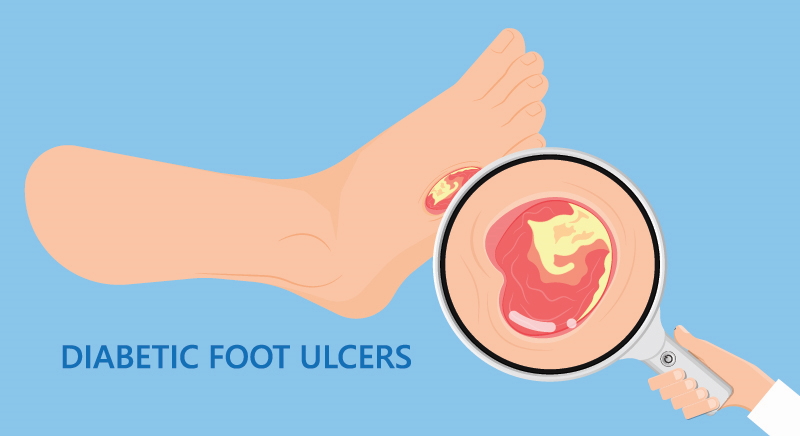
Blood Clots
Over time, chronic diabetes can wreak havoc in the blood vessels, making diabetic patients more susceptible to venous disease. According to the American Heart Association, diabetes increases the risk of blood clots. Up to four in five people with diabetes are at risk of dying from a clot-related cause. They are most common in the legs, as Deep Vein Thrombosis (DVT) or Superficial Venous Thrombosis (SVT).
DVT is a life-threatening condition where blood clots form in one of the veins deep within your body. Swelling only on one side is perhaps the most worrisome sign where you must seek expert vascular care. One-sided swelling may indicate a blood clot or DVT.
One common complication of DVT is known as post-thrombotic syndrome. People with this syndrome may have a swollen leg that feels heavy and hurts. More severe cases of post-thrombotic syndrome can lead to the formation of chronic wounds.
How Can I Reduce My Risk of Diabetic Vascular Disease?
People with diabetes can also reduce their risk of diabetic vascular disease by taking these appropriate steps:
- Avoid high sodium foods (choose high-fiber foods instead)
- Elevate your legs while resting
- Keep the toenails trimmed or ask the doctor to trim them
- Properly manage blood sugar levels at all times
- Avoid smoking
- Stay active with regular exercise or moderate physical activity
- Protect the skin by gently washing and drying your feet daily, then applying lotion
- Manage high blood pressure and high cholesterol
- Drink plenty of water
- Get in the habit of taking supplements and vitamins
- Wear comfortable well-fitting shoes and avoid walking barefoot
- Control your body weight
- Visit your physician or vascular specialist regularly. Follow up with all appointments and instructions.
- If your job requires standing, wear compression socks to boost circulation
- Check daily your feet and legs daily for indicators like swollen veins, skin discoloration, sores, ulcers, etc. Use a mirror to see the bottom of the feet
- Avoid subjecting your feet to extreme temperatures, especially hot water in the bathtub

StrideCare Can Help with Diabetic Vascular Disease
Sadly, so many people think they are stuck with the negative effects of diabetes, and that diabetic vascular disease is part of the territory. But the reality is that diabetes and its symptoms can be managed. Diabetic vascular disease doesn’t have to spell the end of a normal, pain-free life. In many instances, the underlying cause for your diabetic symptoms is vascular related. This can be managed with the appropriate level of care and the right team of vascular specialists in your corner.
StrideCare physicians are board certified diagnostic radiologists with additional fellowship training in vascular and interventional radiology. If you need vascular treatment—or have questions on how to avoid the onset of arterial disease—the experts at StrideCare will recommend an individualized plan to help you get the best results. Request an appointment for a diabetic vascular disease evaluation to discuss your options.
Prior to starting any new treatment or questions regarding a medical condition, always seek the advice of your doctor or other qualified health provider. This information is not a substitute for professional medical advice.
StrideCare serves the South Texas area including Houston, San Antonio, Austin, Round Rock, Bastrop, Brushy Creek, Cedar Park, Converse, Georgetown, Hutto, Kyle, Leander, Marble Falls, New Braunfels, Pasadena, Pearland, Pflugerville, San Marcos, Schertz, Houston, Sugar Land, Katy, Webster, Bay City, Clear Lake, Lake Jackson, The Woodlands, Universal City, Spring, Kingwood, Stafford, Conroe, Texas City, Cypress, League City, Bellaire, and more.