5 Ways To Treat Your Peripheral Artery Disease
Author: StrideCare Internal Team

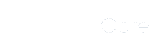
Peripheral artery disease (PAD) is a dangerous condition where plaque buildup on the walls of blood vessels causes them to narrow and leads to poor blood circulation to the kidneys, intestines, arms, legs, and feet. PAD impacts 8.5 million U.S. adults and 113 million people worldwide. And, like many other chronic conditions, the earlier you treat it, the better. That said, peripheral artery disease and the complications that can arise from it are almost always preventable—provided that we are all educated on its warning signs, ways to seek treatment, and lifestyle choices that can help us avoid going down that path.
With September being PAD Awareness Month, our team of vascular, venous, and arterial experts at StrideCare look beyond the minimally invasive PAD treatment options at our Dallas-Fort Worth locations to educate our patients and help them take control of their vascular health. Any significant blockages that restrict blood flow to your limbs or organs can cause irreparable damage over the long term, including issues with gangrene that lead to amputation. And yet, many people simply have not heard of PAD.
What Is PAD?
Simply put, peripheral artery disease—also known as arteriosclerosis, peripheral arterial disease, or peripheral vascular disease (PVD)—is a condition that affects blood circulation in your legs. It occurs when the arteries that supply blood to your legs become narrowed or blocked by plaque. Plaque is made of fatty deposits, calcium, and cholesterol. When these substances harden, a person experiences a wide range of symptoms and becomes at risk for coronary artery disease, heart attacks, or strokes.
The scary part about peripheral artery disease is that while symptoms can vary widely, up to 4 in 10 people don’t even have symptoms at first. Others may have minor leg discomfort or fatigue that is chalked up to osteoarthritis or neuropathy.
Just a few of the PAD symptoms you may experience include the following:
- Painful cramping in the legs or hips, especially while active, but feel better at rest
- Changes in the appearance of extremities (color, loss of hair, shiny skin)
- Cold legs and feet
- Thickening of the toenails
- Open sores that don’t heal
- Dry, scaly, flaky, or leathery skin
- Erectile dysfunction
- No pulse or weak pulse in legs and feet
While anyone can get PAD, it is more prevalent in people starting around age 40 and sharply increasing at 70 and older. Black Americans also have an increased risk of PAD, as do those with poor diet, hypertension, high cholesterol, and a sedentary lifestyle. Approximately 35-55% of patients with PAD also show hypertension, and 80% of patients with PAD are current or former smokers. Not to be outdone, 20-30% of people with PAD are also diabetic.
This is why PAD Awareness Month is important.
PAD is life-threatening if left ignored, misdiagnosed, or unchecked. Ways that healthcare providers and the general public can observe PAD Awareness Month include:
- Increase PAD awareness through articles and resources
- Share common risk factors
- Improve access to PAD screenings and treatments
- Reduce care costs, where possible
- Continue fundraising initiatives
- Encourage someone you know to get checked
- Share stories and testimonials by those impacted by PAD
5 Lifestyle Modifications to Treat or Reduce the Risk of PAD
The good news with peripheral artery disease is that it is treatable. But it is crucial—especially during PAD Awareness Month—to empower people to change their lifestyle habits. Learning how to reduce your risk for PAD is important to remain healthy for years to come. Here are a few suggestions.
Eat a healthy diet
Improving your diet improves overall blood circulation, weight loss, and cardiovascular health. Options include fruits and vegetables, foods high in Vitamin C and E, low-fat dairy and meats, and fiber-rich foods. Also, try to limit saturated fats and avoid trans fats that contain things like hydrogenated vegetable oils.
Exercise and stay active
Our arteries and veins rely on gravity to pump blood throughout our body, and this increases with activity and exercise. For adults, the American Heart Association recommends at least 150 minutes per week of moderate-intensity aerobic activity and increasing the amount and intensity of those exercises gradually over time. We understand walking may be painful if you have PAD, but it’s one of the best things you can do to improve blood circulation to your legs. Try to walk a bit farther each day. Talk to us about treatment if it’s too painful.
Quit smoking
If you smoke, try hard to quit. Smoking causes inflammation in your blood vessels that can lead to blocked arteries. As a result, you’re at a higher risk of having PAD, a heart attack, or a stroke.
Take care of underlying conditions
If you’ve already been diagnosed with high blood pressure, diabetes, or high cholesterol, it’s important to follow your doctor’s advice and take all medications as prescribed. Keeping these health conditions under control lowers your risk of developing PAD.

Keep an eye on your feet
If you have PAD, your toenails may grow at a much slower rate than they used to, and you may have sores that take a long time to heal. Make it a habit to check your feet every day for signs of trouble. Sores can get infected or turn gangrenous if not treated soon enough.
Sometimes, you may need medical help to treat PAD. Depending on the severity of your condition, physicians may prescribe medication like blood thinners to aid blood flow or statins to lower cholesterol.
If necessary, your doctor may suggest minimally invasive treatments to successfully beat PAD. Our vascular experts generally turn to three procedures in these situations.
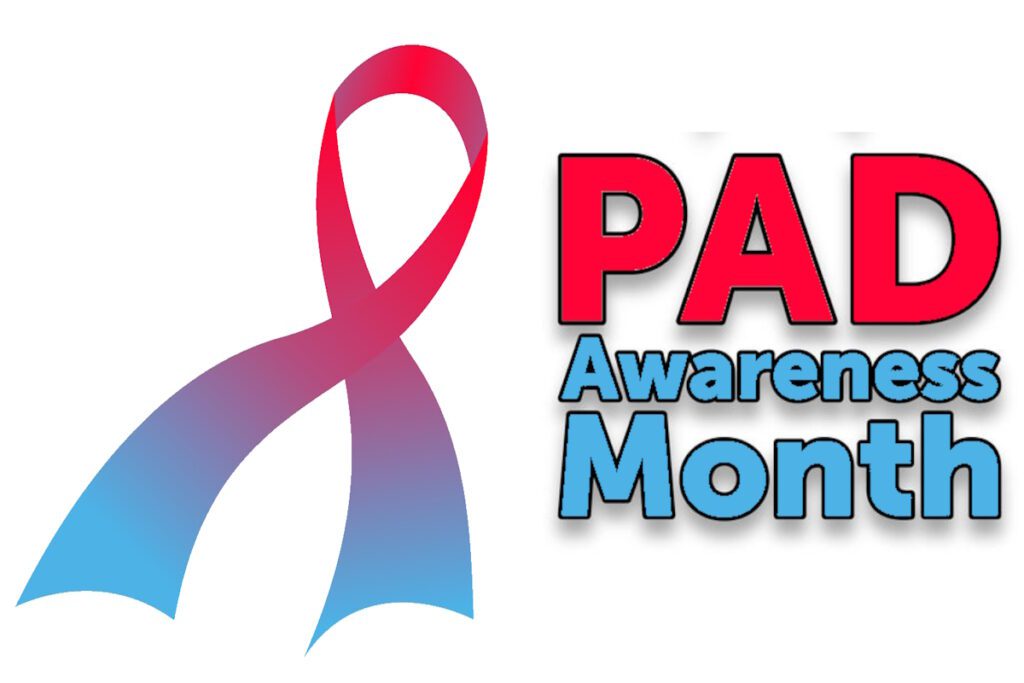
- Angioplasty — A balloon system that uses a catheter to open up narrowed or blocked arteries.
- Atherectomy — Advanced laser technology that clears away built-up plaque on large blood vessels.
- Stenting — This involves a small mesh tube to keep closed-off blood vessels open for the long term.
Spread the Word and Educate Others on Peripheral Artery Disease!
Peripheral artery disease can sound scary, especially when you consider the symptoms you may be facing. But as stated earlier, PAD is highly treatable when caught early, and it is possible for you to lead a normal and healthy life. The good news is that the team of specialists at StrideCare are on the cutting-edge of medicine, helping patients avoid traditionally long invasive surgeries used in the past to treat a variety of conditions to relieve them of their underlying vascular, vein or artery disease issues.
Procedures take place at in-office or outpatient settings. Patients suffering from a multitude of vascular conditions that include venous insufficiency, varicose veins, spider veins, diabetic vascular disease, venous ulcers, peripheral artery disease, leg discoloration, lymphedema, restless legs syndrome, and more can benefit from these minimally invasive treatments.
Prior to starting any new treatment or questions regarding a medical condition, always seek the advice of your doctor or other qualified health provider. This information is not a substitute for professional medical advice.
StrideCare serves the South Texas area including Houston, San Antonio, Austin, Round Rock, Bastrop, Brushy Creek, Cedar Park, Converse, Georgetown, Hutto, Kyle, Leander, Marble Falls, New Braunfels, Pasadena, Pearland, Pflugerville, San Marcos, Schertz, Houston, Sugar Land, Katy, Webster, Bay City, Clear Lake, Lake Jackson, The Woodlands, Universal City, Spring, Kingwood, Stafford, Conroe, Texas City, Cypress, League City, Bellaire, and more.