Is My Leg Swelling from Lymphedema or Chronic Venous Insufficiency?
Author: StrideCare Internal Team

Sue* has never been the type of person who goes to the doctor for what she calls “every little thing.” But she knows the swelling in her legs isn’t normal. For one, the swelling isn’t going away and is getting uncomfortable. And on top of that, there appears to be no rhyme or reason for the condition. No bug bites or injuries, no new medication. After some quick online research, she narrows the possible reasons to lymphedema or chronic venous insufficiency. Both conditions can be life-altering if left unchecked. But which one is it?
While easy to chalk up to injury or an allergic reaction, leg swelling warrants a doctor’s visit. This is especially true if you or your doctor suspect lymphedema or chronic venous insufficiency. While similar in symptoms, these complex conditions happen for different reasons and require dedicated treatments to manage and maintain your health.
Is Lymphedema in Legs a Vascular Problem?
In one word—yes. Our veins carry blood back to the heart to support many systems critical to our cardiovascular health and other functions. Things are great when working properly. But that’s not always the case as we age. Our vein valves can weaken and struggle to pump blood as efficiently as they once did. As a result, blood can pool and accumulate in our bodies.
Lymphedema, also known as lymphatic dysfunction, is a condition that affects up to 10 million Americans. It results from your lymph nodes not draining excess fluids from the fatty tissues just under your skin. Your lymphatic system—a network of lymph nodes, ducts or vessels, and organs—are responsible for carrying this fluid through the body to keep your tissues healthy and give you the ability to fight off infections. When your body can’t properly do this, the lymph fluid collects in one area (often in the arms or legs) and causes swelling.
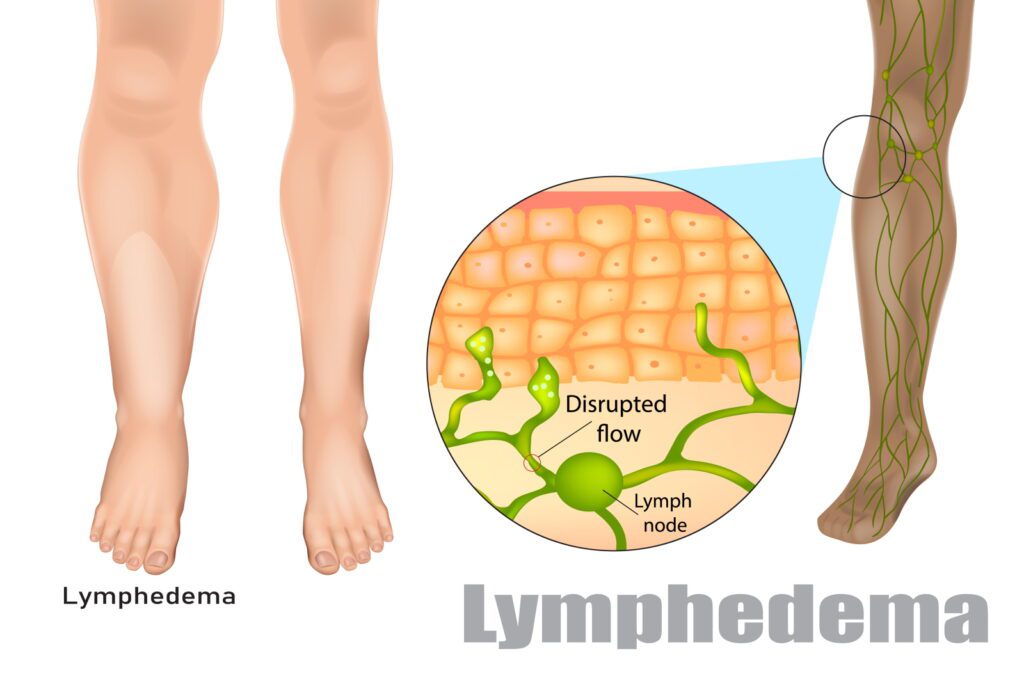
The affected area becomes huge, and skin changes can become permanent.
Lymphedema symptoms include:
- Swelling in the legs, arms, chest, shoulder, etc.
- Changes in the texture of the skin
- Skin discoloration
- Extremities may feel full or heavy
- Aching, tingling, or numbness
- Infected open wounds
- Limited mobility in nearby joints
Who Is Most Likely to Get Lymphedema in Legs?
More people suffer from lymphedema than Multiple Sclerosis, Muscular Dystrophy, ALS, Parkinson’s disease, and AIDS combined. In terms of who is most likely to suffer from it or what it’s caused by, that depends on a variety of factors. We’ve listed a few of them below.
- Genetics
There are two types of lymphedema: primary and secondary lymphedema. While only affecting 1 in 100,000 individuals, primary lymphedema is an inherited or congenital condition that causes a malformation of the lymphatic system. Because of these faulty genes, fluid can’t drain properly or work as they should. Secondary lymphedema is much more prevalent, affecting 1 in 1,000 Americans and can be caused by various things.
- Injury, trauma, or infection
If you were in a car accident and suffered extensive bruising or soft-tissue loss to one area of your body, you are more at risk for developing lymphedema. This is because the lymphatic vessels under your skin have been damaged and cannot circulate the lymph fluid correctly. Additionally, an infection that doesn’t resolve itself quickly or spreads may cause lymphatic system damage to become worse.
- Other health conditions/surgery
Heart and vascular diseases, arthritis, eczema, and cancer are all examples of health-related issues and illnesses that can lead to lymphedema. In situations where cancer surgery is required to remove lymph nodes or some of the vessels that carry lymph fluid can eventually cause fluid buildup. Radiation therapy is often the reason for lymph nodes being damaged, blocked, or scarred.
- Immobility
Individuals who do not move around a lot (example: an elderly individual who is bedridden, extremely sedentary lifestyle, individuals who are bedridden because of injury or illness) run the risk of developing secondary lymphedema because their body doesn’t have a chance to drain excess fluid.

How is Chronic Venous Insufficiency Similar or Different?
Much like lymphedema, chronic venous insufficiency (CVI) happens when your body cannot correctly circulate fluid. But the fluid related to CVI is your blood, not lymph fluid. Also, your lymphatic system is not the problem—it’s your veins. Your veins typically work on a one-way system using a series of solid valves to ensure the traveling blood doesn’t flow back in the opposite direction with gravity. As we age, our veins become weaker and can be affected by life choices such as diet, excess weight, smoking, and a sedentary lifestyle.
As a result, weak valves in the veins can lead to blood pooling in areas it shouldn’t and creating a variety of complications and discomfort. Chronic venous insufficiency is characterized by broken vein valves that no longer hold a proper seal. As a result, poor blood flow from the veins in your legs back up to your heart will cause blood to pool in your legs. This can cause a variety of issues, including:
- Swelling in the legs only (lymphedema also affects feet)
- Dull aching, cramping, tingling, or numbness
- Changes in the texture and color of the skin
- Varicose veins
- Pain that worsens when you stand

Does a Vascular Doctor Treat Lymphedema and CVI?
Yes! Our team at StrideCare offers personalized treatments for a variety of vascular conditions, including lymphedema and chronic venous insufficiency. The first step is always to schedule an appointment to receive a timely diagnosis through ultrasound and other tests. While lymphedema may not be life-threatening, it can be extremely uncomfortable for our patients.
We are proud to offer personalized lymphedema therapies to help our patients get back to the healthiest version of themselves. Examples of lymphedema treatment include therapeutic wrapping or bandaging to encourage lymph fluid circulation. Some patients may also benefit from incisions and drainage procedures to relieve fluid buildup in a swollen and infected patch of skin. Minimally invasive and microsurgeries also provide relief without needing invasive surgeries.
Chronic venous insufficiency requires a slightly different set of minimally invasive treatments, including Microfoam Ablation, Radiofrequency Ablation (RFA), Sclerotherapy and other vein treatments.

Lymphedema and CVI: StrideCare Can Help!
Sometimes, swelling of the legs and feet is nothing to be overly concerned about. This is especially true if the swelling subsides after a short period and isn’t accompanied by any significant pain. But at StrideCare, we believe in promoting education and awareness efforts aimed at letting people know that chronic leg swelling can also be a sign of a more serious condition such as lymphedema or chronic venous insufficiency. These changes are your body’s way of telling you something is wrong. Ignore them, and you could drastically impact your quality of life.
In many instances, the underlying cause can be managed with the appropriate level of care and the right team of vascular specialists in your corner. StrideCare physicians are board certified diagnostic radiologists with additional fellowship training in vascular and interventional radiology. If your legs need treatment—or you have questions on how to avoid the onset of vein disease—the experts at StrideCare will recommend an individualized plan to help you get the best results. Request an appointment for a vein disease evaluation to discuss your options.
Prior to starting any new treatment or questions regarding a medical condition, always seek the advice of your doctor or other qualified health provider. This information is not a substitute for professional medical advice.
StrideCare serves the South Texas area including Houston, San Antonio, Austin, Round Rock, Bastrop, Brushy Creek, Cedar Park, Converse, Georgetown, Hutto, Kyle, Leander, Marble Falls, New Braunfels, Pasadena, Pearland, Pflugerville, San Marcos, Schertz, Houston, Sugar Land, Katy, Webster, Bay City, Clear Lake, Lake Jackson, The Woodlands, Universal City, Spring, Kingwood, Stafford, Conroe, Texas City, Cypress, League City, Bellaire, and more.
*Patient stories are true. Names and/or photos may be changed to protect patient confidentiality.